Wireless LED Device Fights Deep-Seated Cancers With Light
Insights | 30-07-2024 | By Robin Mitchell
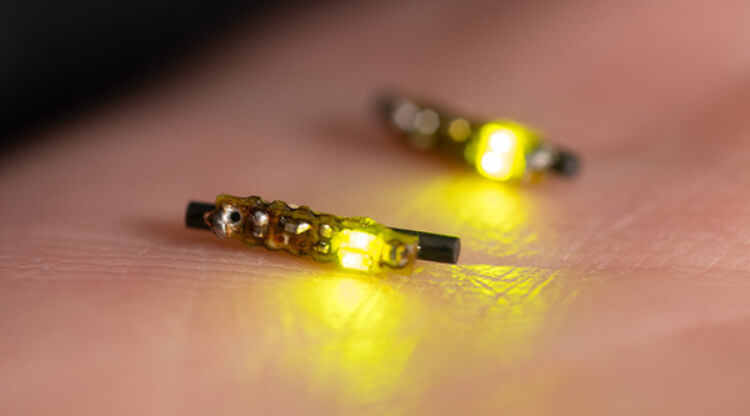
A miniature, implantable LED device combats cancer using light.
In medical technology, a groundbreaking innovation has emerged with the development of a rice-sized LED device designed to combat deep-seated cancers using light. This cutting-edge technology represents a significant advancement in the fight against cancer, offering a minimally invasive approach to targeting tumors. As researchers prepare to move forward with testing this novel device on mice, the potential implications for the future of cancer treatment are profound.
What challenges does the detection and treatment of cancer present, what are the anticipated benefits of its minimally invasive nature for patients undergoing treatment, and how might this innovative approach transform current cancer therapy practices?
Key Things to Know:
- Groundbreaking LED Device: A rice-sized LED device has been developed to combat deep-seated cancers using light, offering a minimally invasive approach to targeting tumours.
- Enhanced Immune Response: The device not only targets cancer cells but also mobilises the body's immune system, creating a dual-action attack against tumours.
- Potential for Human Trials: While currently being tested on mice, the device shows promise for human trials, potentially becoming a future standard of care in oncology.
- Reduced Side Effects: This innovative approach could reduce side effects associated with traditional treatments, such as chemotherapy, and improve patient mental health during treatment.
Cancer's Invisible Enemy: The Complex and Multifaceted Nature of the Disease
Despite the many advances in medical science, the detection and treatment of cancer remains a major challenge for the medical community. When it comes to detecting cancer, doctors face a multitude of challenges, as many cancers are effectively invisible to medical imaging technologies.
For example, breast cancer can begin as a single cell that multiplies and forms a large tumour, but it is only when a mammogram detects a change in density that its presence can be confirmed. Even then, such imaging technologies are not able to distinguish between cancerous and non-cancerous tissue, meaning that biopsies are often needed to confirm a diagnosis. Other cancers, such as those found in the stomach and oesophagus, cannot even be seen via internal imaging technologies, meaning that their presence can only be confirmed after symptoms show.
One innovative approach to overcoming these challenges is the development of advanced diagnostic devices, such as the implantable LED device, which uses specific types of light to target and destroy cancer cells. By integrating light-sensitive dyes and leveraging the body's immune response, these devices offer a new avenue for detecting and treating cancers that are otherwise difficult to identify and manage.
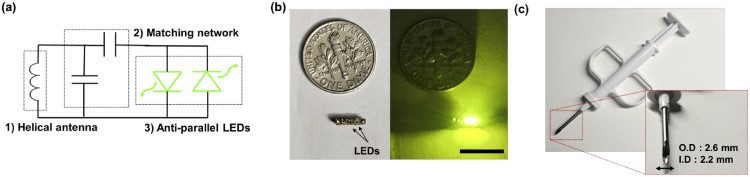
Fig. 1. (a) Diagram of the LED device. (b) Size comparison with a US dime (scale bar: 10 mm). (c) The device shown fitting inside a 12 G biopsy needle.
Challenges in Detecting and Treating Cancer
This complexity is further compounded by the fact that cancer is a multifaceted disease posing a major health challenge worldwide. The resistance of cancer cells to treatment is one of the primary reasons for the failure of cancer therapy. While initial treatment may be effective in eliminating the tumour, cancer cells can develop resistance to chemotherapy and other treatments over time, making them difficult to manage and eliminate. This resistance can develop through various mechanisms, including the ability of cancer cells to repair DNA damage, produce protective molecules, and form new blood vessels that supply them with nutrients and oxygen.
The heterogeneity of tumours also presents a major challenge in cancer management. Tumours are composed of different types of cancer cells, each with unique characteristics and responses to treatment. This heterogeneity can make it challenging to identify the most effective treatment strategies and target specific cells. Furthermore, the heterogeneity of tumours can also lead to the development of new cancer cells that are resistant to treatment, thus limiting the efficacy of current therapies.
But above all else, one of the most significant challenges in cancer treatment is the metastasis of cancer cells from the primary tumour to other parts of the body. Metastatic cancers are difficult to treat and have a poor prognosis as they can spread to various organs, including the liver, lungs, and brain. The process of metastasis is complex and involves the ability of cancer cells to break away from the primary tumour, enter the bloodstream or lymphatic system, and travel to distant sites in the body.
The Impact of Metastasis and Treatment Side Effects
The side effects of cancer treatments can also have a major impact on a patient's quality of life. While treatments such as chemotherapy can help to eliminate cancer cells, they can also cause significant toxicity to normal cells, leading to hair loss, fatigue, nausea, and vomiting. These side effects can be severe enough for patients to discontinue their treatment, thereby reducing the effectiveness of cancer therapy.
The psychological impact of a cancer diagnosis can also be debilitating for patients. The stress and anxiety related to treatment, the possibility of recurrence, and the impact on daily life can affect patients' mental well-being and their ability to cope with treatment. The emotional burden of a cancer diagnosis can also affect patients' relationships with family and friends, leading to feelings of isolation and distress.
A New Lens on Cancer Treatment
The development of a rice-sized LED device could usher a new era in cancer treatment as researchers look to harness the power of light to target and destroy deep-seated cancers. Unlike traditional treatments, this device provides a minimally invasive alternative, potentially reducing the need for more aggressive methods and improving patient outcomes.
Researchers at the University of Notre Dame have highlighted that certain types of light, particularly green light, can penetrate tissue more effectively, offering a robust response against cancer cells. This innovative approach not only targets the cancer cells but also mobilises the body's immune system, creating a dual-action attack against the tumour.
While the device has yet to be tested on mice, the results of these experiments could pave the way for a paradigm shift in oncology. By shining light on cancer cells, the device takes advantage of the sensitivity of some cells to light, specifically those that contain non-repeating structures such as melanin.
Potential Breakthroughs in Light-Based Cancer Treatments
The device's ability to induce pyroptosis, a type of cell death known to trigger a strong immune response, is particularly promising. This method could lead to a cascading effect, where the immune system is trained to recognise and attack other cancerous cells, potentially preventing the spread of the disease.
If the device proves to be effective in mice, the next step would be human trials, and if these are also successful, the device could become a standard of care in the future. The ability to target cancers with accuracy and precision could reduce side effects associated with other treatments, such as chemotherapy, and the use of light could help to improve patient mental health during treatment.
The use of biologically safe light could also reduce the risk of secondary cancers caused by radiation therapy. However, the device may not be able to eliminate all cancers, and some may require a combination of the device and other treatments.
Moreover, the wireless nature of this LED device allows for real-time monitoring and adjustments during treatment, enhancing the precision and effectiveness of the therapy. This feature could be particularly beneficial in tailoring treatments to individual patients, ensuring that each session is optimised for the best possible outcome.
The Future of Cancer Therapy
The use of a rice-sized LED device to target and destroy deep cancers could usher in a new era of cancer therapy. If successful, this technology could shift the paradigm of cancer treatment towards more targeted and less invasive therapies, reducing treatment side effects and improving the quality of life for patients. By utilising light to destroy cancerous cells, this approach also has the potential to minimise the impact on daily life during treatment, something that is often a major concern for patients undergoing therapy.
The minimally invasive nature of the device allows for precise targeting of cancerous cells, leading to fewer side effects compared to traditional treatments. This reduction in side effects also reduces the physical and emotional burden on patients, something that is often severe. Furthermore, this technology has the potential to lower production costs, making advanced cancer treatments more accessible to a wider population, thereby democratising cancer care.
The precision offered by this innovative approach also has the potential to enhance precision medicine, tailoring therapy to the specific characteristics of a patient's tumour. By optimising treatment outcomes and minimising the risk of recurrence, healthcare providers can improve the effectiveness of cancer therapy and provide more individualised care. This patient-centric approach to medicine also has the potential to improve communication between healthcare providers and patients, leading to better health outcomes and higher patient satisfaction rates.
As this technology continues to evolve, engineers and researchers will play a crucial role in advancing our understanding of light-based cancer treatments. The successful translation of this technology into real-world clinical practice will require collaboration between engineers, clinicians, and researchers from various fields, highlighting the power of interdisciplinary approaches in medical innovation. Ultimately, the integration of this LED technology into cancer therapy could lead to new insights into the role of light in human health and disease, pushing the boundaries of medical science forward.

