Blood Sweat and Saliva Analysis: Next-Gen Medical Sensors
Insights | 16-01-2025 | By Gary Elinoff
Key Takeaways about Blood Sweat and Saliva
- Garnering medical information from blood, sweat, or saliva involves a synergy between electronics and biochemistry.
- Medical Sensors based on blood, sweat, and saliva speed up testing and make it less dependent on expensive centralized medical testers.
- Point of care devices (POC) make it possible to obtain measurements of critical biomarkers continuously, as the subject goes through the ordinary stresses of daily life. This knowledge may be far more valuable then static measurements made in a clinical office.
Introduction
One of the things to know about Medical electronic sensors is that here, electronics have a costar in biochemistry. There are far to many to cover them all in one short summary, but examining even a small sample is eye opening.
In some cases, they are based on one-time-use test cards that require no special care or refrigeration. These cards contain within themselves the means to execute complex chemical tests for biomarkers, and the tiny samples are fed by special microfluidic channels (more about them later) that are a wonder in themselves.
Other types use the presence of a test for antigens to change the capacitance between electrode pairs. This change is sensed and measured by ultra-miniature electronic circuitry. The results are displayed almost immediately to healthcare providers, who can now make decisions in minutes, not hours, with potentially lifesaving results.
Electronic Blood Analysis
Modern systems for electronic blood analysis can deliver complete results at a low cost, and they can do so in minutes rather than in hours. Siemens' EPOC[1] is a handheld system that is purposed to point care testing (POCT). With POCT, tests can take place anywhere the patient happens to be at any point in time, with no reference to a remote, overburdened central laboratory.
One of the thirteen tests that the Siemens system can perform is an analysis of lactic acid, a key indicator for sepsis. As described by healthcare workers at Huntsville Hospital, an extremely fast turnaround for sepsis testing is vital because mortality rates for sepsis increase dramatically for every minute waiting for test results. The hospital reports that classical sepsis testing takes at least 30 minutes, and that's only if the test is performed on a "stat" basis and if everything goes smoothly. With Siemens' system, after a minute or two of initialization, results can be reported in only one minute.
As illustrated below, Siemens' EPOC system consists of three main components: left to right, the host, the reader, and the test card. In a typical application, the patient care operator first initializes the host and inserts the Test Card. Then, a tiny blood sample of 92 microliters is delivered to the card. Analysis takes about 60 seconds, with the results displayed in the reader for immediate results, although the reader can, of course, communicate with remote logging systems. The test cards do not need to be refrigerated.
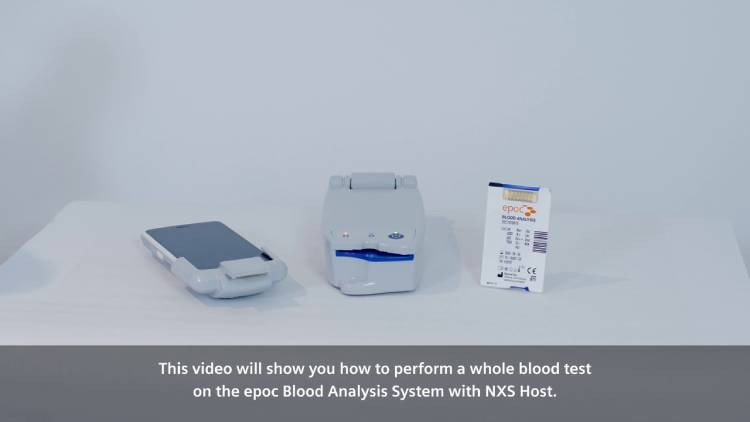
Image source: Siemens' Performing a Whole Blood Test Video 0:14
The system can measure the following vital clinical indications:
- pH
- pCO2
- pO2
- TCO2
- Sodium
- Potassium
- Ionized Calcium
- Chloride
- Hemocrit
- Glucose
- Lactate
- BUN/Urea
- Creatine
Once the blood sample is introduced, the main action takes place, all within a minute, in the Test Card. And what action it is! The Test Card is a disposable chem lab, complete with everything needed to detect and quantify, separately, the 13 key parameters listed above. For those who flex their chemistry muscles, Siemens offers descriptions of the complex chemical "nuts and bolts" of how each of the thirteen tests is accomplished and talks about miniaturization!
Saliva Reveals Its Secrets
Researchers from the University of Florida and National Yang-Ming Chiao Tung University in Taiwan have developed a handheld device that can detect breast cancer from a drop of saliva. Best yet, as reported via AIP Publishing[2], it's based largely on widely available test strips, open-source software and inexpensive electronic components.
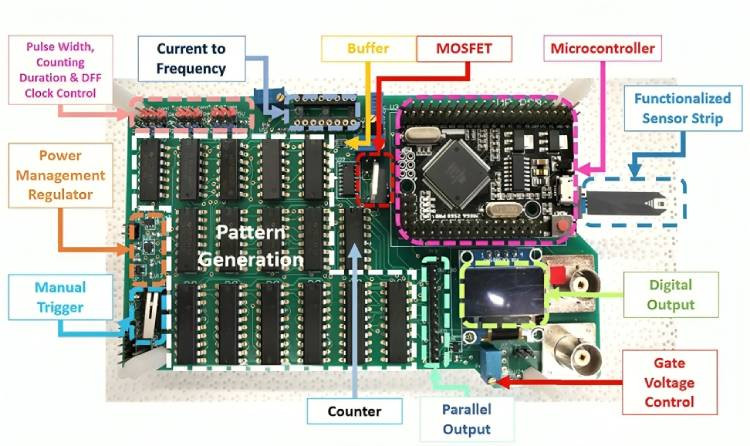
Image source: AIP
It starts with a sensor strip that contains antibodies targeted at the cancer biomarkers. After the saliva sample is placed on the strip, the device then zaps it with electrical pulses. This causes the biomarkers, if they are present, to bind with the antibodies. The binding alters the charge and capacitance of an electrode, signaling a dreaded diagnosis.
The article doesn't indicate that this particular application is ready for prime time in advanced nations, but as per one of the study's authors, Hsiao-Hsuan Wan, "In many places, especially in developing countries, advanced technologies like MRI for breast cancer testing may not be readily available," furthermore "Our technology is more cost-effective, with the test strip costing just a few cents and the reusable circuit board priced at $5. We are excited about the potential to make a significant impact in areas where people might not have had the resources for breast cancer screening tests before."
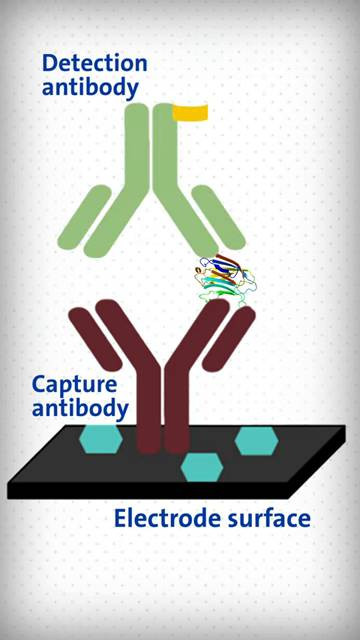
Antigen caught between Capture and Detection Antibody Causes current to flow, indicating its presence source: LabMedica Video 0:31
Sweat offers Non-Invasive Access to critical Biomarkers
Human sweat offers a wealth of insights into human health. A key advantage over blood-based analysis is that there is no need for invasive and potentially dangerous blood draws. And, while accessing saliva isn't dangerous, many patients will find providing saliva to be an unpleasant and undignified experience. But because everyone sweats to some extent, sweat analysis stands out as a great non-invasive modality. As it turns out, fingertips produce a disproportionate amount of sweat relative to their size, making fingertips a great site for this type of analysis.
Illustrated below, researchers at the University of California have developed a "finger wrap" [3] that monitors bodily levels of glucose, lactate, vitamin C and levodopa.
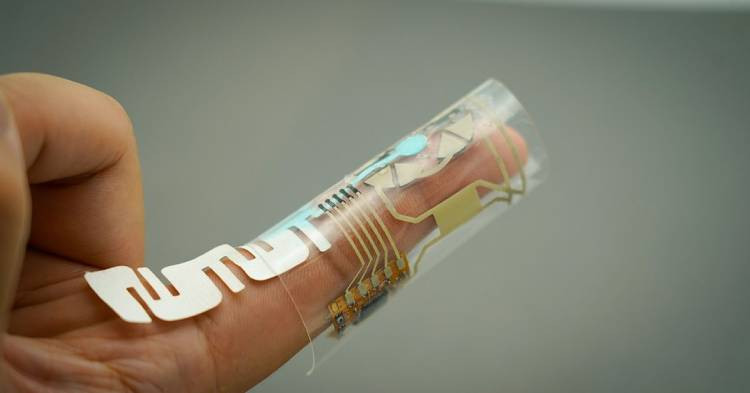
Powered by the wearer’s fingertip sweat, this finger wrap simultaneously measures glucose, lactate, vitamin C, and levodopa levels in that same sweat. Credit: Shichao Ding.
As depicted above, "The device is constructed from several electronic components printed onto a thin, flexible and stretchable polymer material. Its design allows it to conform to the finger while being durable enough to withstand repeated bending, stretching and movement. "
Interestingly, the sweat itself is a source of the minuscule amount of power needed to power the device. This is achieved through the employment of biofuel cells, designed specifically to collect chemicals present in sweat and convert those chemicals into electricity. The electricity thus garnered is stored in onboard silver chloride-zinc batteries.
The sweat to be analyzed transits through tiny paper microfluidic channels to the four sensors, one each for each of the four bodily markers being measured. There is also a bluetooth low energy transmitter that transmits the analytical results to external receivers, where the results can be read and stored. The "finger wrap" is entirely self-contained, powered entirely by biofuel cells' energy, stored in the silver chloride-zinc batteries.
Challenges and Opportunities
One of the major challenges for these newer types of medical electronic sensors is building trust. Many of these devices are not certified by the appropriate bodies, with researchers and clinicians alike wary of trusting them. A clear demarcation must be made between things like devices for phys ed buffs to chart their courses, to solid devices on which medical providers to use to make decision on which YOUR LIFE may depend.
Another challenge is security because for these devices to fully live up to their potential, they must transmit results and findings over the IoT. Ultimately, they'll need to provide for the encoding of results to protect patient privacy. And they must also be protected against hacking, as bad actors may well be able to benefit from providing false information to subjects and their medical providers.
Wrapping Up
These biomarker readings are important additions to patient medical records. Additionally, patients' biological records, taken while they are out of the hospital and leading mostly regular lives, will be of enormous value to medical researchers.
For these reasons and many more, even though these devices are designed to give doctors IMMEDIATE results so that they can make life or death decisions Right Now, these invaluable insights must be uploaded to servers where they can be analyzed and learned from.
This happens through the many forms of the Internet of Things (IoT). Electropages' article, "Remote Health Monitoring Courtesy of the Internet of Things", will be of interest here.
And finally, one of the major focuses of "computer" technology is to localize as much as possible. Decisions are made and carried out close to the action as practical. Results are uploaded largely for strategic decisions, research and record-keeping. These similarities, in addition to the emphasis on miniaturization, indicate that medical medical technology is following a similar path.
References:
- Raising the benchmark for handheld blood gas testing again. Siemens
- Would You Prefer a Mammogram, MRI, or Saliva on a Test Strip? AIP Publishing (American Institute of Physics)
- Finger Wrap Uses Sweat To Provide Health Monitoring at Your Fingertips—Literally. University of California San Diego
Glossary of Terms
- Point Care Testing (POCT). A diagnostic test performed near the patient, often in an emergency room or at bedside.
- Microfluidics. The technology of tiny amounts of fluids flowing through channels measuring as small as tens of micrometers in size. Fluid volumes of 10-9 liters and even smaller can be manipulated, making this technology extremely important for medical and chemical testing.

