3D Printing Custom Ocular Prostheses: New Tech Insights
16-04-2024 | By Liam Critchley

Key Things to Know:
- Customisation is Key: Each ocular prosthetic must be individually tailored to fit the unique eye socket shape and appearance of the patient, enhancing both functionality and aesthetics.
- Technological Advancements: Recent integrations such as Optical Coherence Tomography (OCT) have significantly enhanced the design process, enabling highly accurate replications of the eye's topography and colouration.
- 3D Printing: Additive manufacturing has brought significant improvements in the production of ocular prosthetics, offering more consistent quality and the possibility of complex, customisable designs.
- Clinical Validation: Studies, including those conducted by Moorfields Eye Hospital NHS Foundation Trust, have confirmed the effectiveness of digitally designed prosthetics in improving patients' quality of life.
The loss of an eye or severe damage to an eye can lead to the need for an eye prosthetic. Technically known as an ocular prosthetic, around 0.1% of the world’s population wears a prosthetic eye today. There are many ways that eyes can become damaged, from trauma to painful blind eyes and eye tumours that cannot be treated. The difference in everyone’s eye structure means that each eye prosthetic needs to be customised to the patient. Damage to the eye leads to a visible difference in a person’s appearance, so while a prosthetic doesn’t add any visible function/restore eye function, it can bring some piece of mind to patients as their new eyes provide aesthetic benefits.
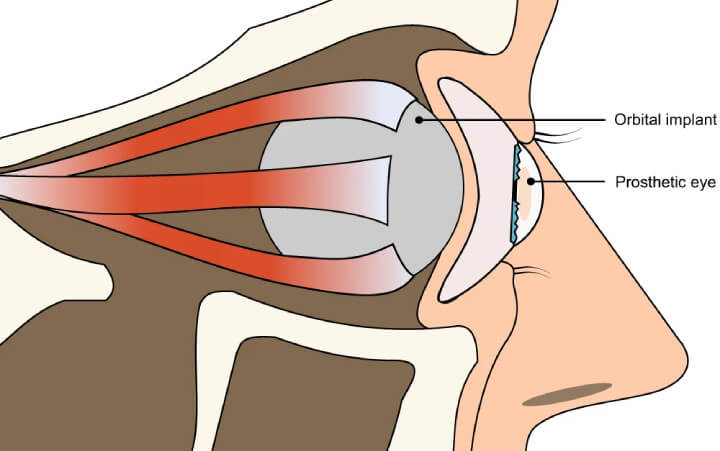
Eye prosthetics are worn over the conjunctiva in the eye and are held by the eyelid. The movement of the implant is possible due to the action of the extraocular muscles. The prosthetic needs to fulfil a number of requirements, including replacing the orbital volume of the eye and providing an acceptable level of comfort to the patient. The prosthetic also needs to be made before the eye socket heals.
Understanding Orbital Implants and Prosthetic Eyes
In cases of enucleation or evisceration—where an eye is removed due to damage or disease—an orbital implant is often used as a foundation within the eye socket. This implant is carefully attached to the eye muscles and is designed to be covered by the conjunctiva, serving as a stable base for the prosthetic eye. The prosthetic itself is positioned between the eyelids and over the implant, allowing for natural movement. This mobility is primarily due to the slight friction between the prosthetic eye and the smooth surface of the orbital implant, which helps to mimic the natural motion of an eye, providing not only cosmetic restoration but also some degree of functional normalcy.
Advancements in Ocular Prosthetics
A significant shift has been observed with the integration of Optical Coherence Tomography (OCT) in the design of ocular prosthetics. This technology aids in accurately capturing the topography of the eye socket and the detailed colouration of the existing eye, which ensures that the prosthetic eye matches the patient's original appearance as closely as possible. This technological advancement supports both aesthetic and functional needs by ensuring a high degree of customisation.
The customised nature of ocular prosthetics means that there are only certain processes available for making them, as the prosthetic needs to match the patient’s eye socket shape and eye appearance. While there are stock prosthetic eyes available, the customised ones are currently produced by highly skilled ocularists. Because these processes rely on human expertise, the quality of the prosthetic is reliant on the craftsmanship of the ocularist, so the quality of the prosthetic can vary from ocularist to ocularist.
Recent developments have showcased the use of automated, data-driven design processes in the creation of ocular prosthetics. These methods utilise advanced imaging techniques to produce a digital model of the prosthetic that perfectly fits the patient’s eye socket, significantly reducing the variability seen with manual craftsmanship and enhancing the prosthetic's functional efficacy.
Being able to digitise and make the process possible with machines while retaining the ability to have a high degree of customisation is sought after. This is where additive manufacturing can come in because it offers a high degree of design freedom and can create complex, customisable parts. The use of additive manufacturing has been growing in the medical sector, and many parts made today are biocompatible and suitable for clinical use. There are many implantable medical devices that have been created with additive manufacturing, and eye prosthetics are one of the latest areas to get the 3D printing treatment.
The use of full-colour 3D printing technologies not only streamlines the manufacturing process but also improves the cosmetic and functional outcomes of ocular prosthetics. By employing a multi-material printing approach, prosthetics can now feature realistic textural gradients and colour transitions that mimic the natural appearance of the human eye, enhancing the prosthetic's integration and the wearer's confidence.
Current Approaches for Ocular Prosthetics
As it stands, current manufacturing methods use artisan crafters who create custom prosthetics through skilled manual labour. The common material of choice for hand-crafting prosthetics is polymethyl methacrylate (PMMA). This process requires the ocularist to take an alginate impression of the patient’s eye socket to cast a wax shape that fits into the socket. The iris is then painted onto a flat disc and embedded into the wax alongside a clear PMMA cornea unit. This process takes around 2 hours with the patient in the clinic, and the wax model needs to be cured for 6 hours as well. After curing, the prosthetic is polished, and any shape adjustments are made at this stage. The whole process takes over 8 hours of manual labour to make a prosthetic with varying degrees of quality and patient compatibility.
Another less commonly used method is the glassblowing of white cryolite glass and coloured glasses to create the iris and veins. This prosthetic is made by manipulating the heated glass, but the fit and appearance of the prosthetic are assessed after it has cooled. The result is that the prosthetic looks more lifelike than a PMMA prosthetic, but it can’t be adjusted to fit the patient’s eye socket after it has cooled. Additionally, because they are made of glass, they get damaged and break more frequently, so they have to be replaced more often.
Turning to Additive Manufacturing for Printing Ocular Prosthetics
Additive Manufacturing has gained a lot of interest in applications where customisability is a key factor. This has included medical devices, such as stents, ball and socket prosthetics, and other joint prosthetics. The shape and material properties of ocular prosthetics is key for the functional side of the prosthetic, but the appearance plays a role from a personal perspective.
Improvement in Prosthetic Functionality
The integration of digital workflows has notably improved the functional attributes of ocular prosthetics. The precise mapping of anophthalmic socket topography allows for a more accurate fit, which significantly enhances comfort for the wearer and optimises the prosthetic's functional longevity by minimising potential issues related to socket fit.
Various 3D printing approaches have been proposed for eye prosthetics, but many of the approaches to date have not used a digital, automated, and data-driven design process that considers both shape and appearance. Instead of an automatic shape prediction, the shapes of the prosthetics are typically designed in CAD or other 3D modelling software.
Researchers have now developed a 3D printing approach, using an automatic, digital end-to-end process to design the prosthetic before printing. The approach uses minimally invasive optical coherence tomography (OCT) to capture the topography of the anophthalmic socket, as well as the anatomy and colouration of the normal eye. After designing, the prosthetic is printed using a multi-material 3D printer.
The automated design approach uses a statistical shape model to predict and best fit the prosthetic shape based on incomplete surface information of the eye socket. A colour-characterised image of the healthy eye was used to generate an appearance of the prosthetic eye that directly matched the original eye, and a full-colour 3D printer was used to bring the aesthetic appearance to life.
Innovations in Prosthetic Design: A Closer Look at the Digital Process
To better understand the cutting-edge technology behind ocular prosthetics, let's delve into the digital design process that has modernized the way these devices are created. Fig. 3 below illustrates the comprehensive data-driven design software process employed to develop each custom prosthetic model. This process integrates detailed anatomical data with technological precision, ensuring each prosthetic is not only aesthetically pleasing but also perfectly matched to the patient’s physical conditions.
Digital and 3D printing technologies have transformed the field of ocular prosthetics by making them more accessible and tailored to individual needs. The ability to generate detailed colour and structural definitions ensures that each prosthetic eye can be customised not just for fit but also for aesthetic nuances, closely replicating the patient’s natural eye.
The process of the digitally designing and 3D printing the prosthetics was also demonstrated in a clinical trial in conjunction with Moorfields Eye Hospital NHS Foundation Trust. 10 clinical patients took part in the study and looked at the long-term impact and performance of the 3D printed prosthetics compared to traditionally crafter prosthetics.
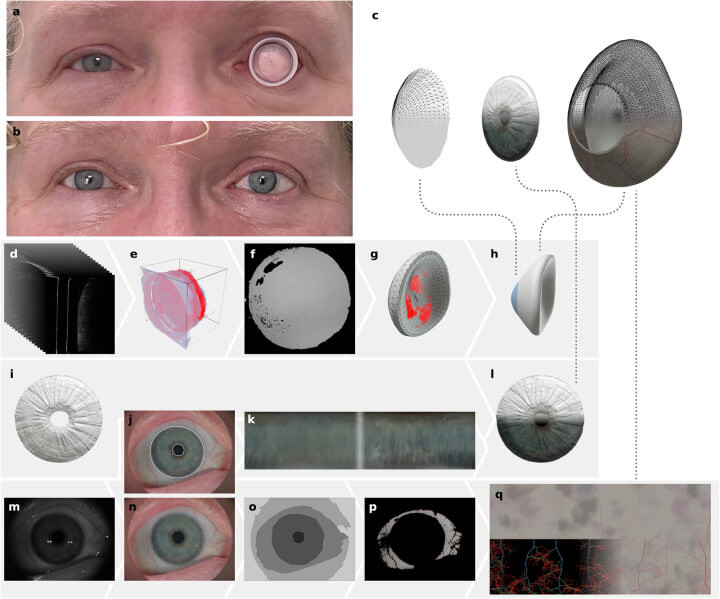
a Patient 5 wearing a conformer fitted inside the eye socket. b Image of Patient 5 showcasing the 3D-printed prosthetic for the left eye (pictured on the right). c An expanded view of the 3D prosthetic model. d–h Steps involved in Shape Prediction: Initial OCT scans of the eye socket (d), volume data filtered to reveal the socket surface (e), transformation of data into a depth map for alignment (f), fitting of the shape to the socket surface (g), followed by smoothing and refining the geometry (h). i–l Process of Iris Creation: The iris geometry captured by the OCT (i), detection of iris and pupil boundaries (j), enhancement of the iris texture for better contrast (k), and standardisation and UV mapping of the iris geometry (l). m–q Development of Colour Image and Sclera Texture: The original colour image (m), enhanced and clarified image post-characterisation and denoising (n), segmentation using the watershed technique (o), vein removal for clearer sclera colour extraction (p), initial and final renderings of the staining texture and the developed veining network (q, left and right respectively).
Proven Efficiency and Benefits in Clinical Trials
While one of the benefits of the digital design 3D printing process is that it requires five times less labour than the ocularist and produces reproducible output, other benefits have been found throughout the study.
First, the colour-calibrated printer enabled the researchers to create prosthetics in which the colour, size, and structure of the iris, as well as the appearance of the sclera, were replicated close to the original eye. Second, the use of 3D printing allows for prosthetics to be printed anywhere there is a suitable printer, so prosthetics could be supplied to areas where services are not readily available.
The 3D printing approach also allows for a very consistent output compared to the manual labour approach, which will enable more accurate spares to be produced when prosthetics get damaged. Manual spares will often be different from the original prosthetics, which can cause complications. The 3D printing approach also negates the need for alginate impressions, as the socket shape is scanned optically.
Finally, the digital workflow used enabled continuous improvements to the prosthetics for all the patients without the ocularist requiring extra training. The combination of more data, the ocularist's expertise, and the patient’s feedback enabled the software to be refined so that it could continuously produce better shapes and replicate distinct features of the eye.
Switching to a digital workflow with 3D printing could enable patients—such as children—who are traditionally not eligible for prosthetics to be now eligible. While this automatic end-to-end approach has been used so far to design and manufacture custom aesthetic eye prostheses, the ability to factor in both shape fitting and aesthetic design could open up the approach to other aesthetic prostheses, such as dental restorations or facial prostheses, as well as covers for more traditional prosthetics that match the patient’s appearance.
Clinical Validation
The recent clinical trial conducted in association with Moorfields Eye Hospital NHS Foundation Trust validates the practical efficacy and the enhanced quality of life provided by these digitally created prosthetics. Patients have reported high satisfaction with the cosmetic accuracy and comfort of their new prosthetics, underscoring the importance of integrating advanced manufacturing technologies in medical applications.
Reference:

